A scoping review of internet access, digital literacy, and health outcomes in adults with Type 2 diabetes
MF: https://orcid.org/0000-0003-0989-2968
Farmer, M.S. (2025). A scoping review of internet access, digital literacy, and health outcomes in adults with Type 2 diabetes. Stacks Journal: 25004. https://doi.org/10.60102/stacks-25004

Abstract photo. Percent of self-reported broadband internet adoption by household, county level (Source: American Communities Survey 2021)
Abstract
Objective
The aim of this scoping review is to synthesize and review current evidence of how Internet availability, Internet adoption, digital literacy, and digital health services affect health outcomes in adults with Type 2 Diabetes.
Methods
The scoping review includes peer-reviewed articles published in English in the last 10 years including CINAHL, PubMed, and Scopus databases. Studies that met inclusion criteria were abstracted into a literature review matrix summarizing key findings and themes. Protocol pre-registered and available here.
Results
The 27 studies meeting inclusion criteria indicate a limited and heterogenous understanding of how digital inequities affect diabetic health. A few themes emerged including: (1) Higher educational attainment and higher income positively impacts rates of Internet adoption, (2) older adults and rural inhabitants face disadvantages in managing diabetes due to poor Internet adoption and limited digital literacy, and (3) many populations are willing and ready to use mHealth applications, independent of their ability to use the Internet. Evidence directly linking Internet adoption to diabetes prevalence in the United States was present in one study published in 2014.
Discussion and Conclusion
Internet and digital inequities can negatively impact knowledge and management of Type 2 diabetes due to barriers in accessing healthcare services, digital self-care management resources, and education published online. The direct effects of Internet availability, Internet adoption, and digital literacy on diabetes outcomes are underexamined. Current population-level data examining the relationships between these factors is warranted.
Keywords: diabetes mellitus, digital equity, Internet, scoping review
Introduction
Background
In 2021, the World Health Organization published a global strategy urging Member States to utilize and expand digital health technologies in ways that provide health services to all in equitable, affordable, and sustainable ways (1). As pressures of the global healthcare worker shortage continues, this call to action highlights the need for populations to be connected to digital health resources (2,3).
In the United States, those experiencing poverty, the elderly, residents in rural areas, and racial/ethnic minorities do not have equitable availability to the Internet and technology due to the intentional withholding of affordable services and lack of investment in high-speed internet infrastructure in low-income communities by Internet Service Providers, also known as digital redlining (4–7). Even with Internet availability, adoption of the Internet and related technologies is limited due to barriers in affordability, perceived value, and low digital literacy (8). For populations burdened with chronic diseases, such as Type 2 diabetes (T2D), inadequate digital health care availability may have a negative impact on health outcomes (9). However, the effects of limited Internet and technology availability and adoption on health outcomes are not well known. The aim of this review is to understand the current knowledge of how Internet or technology availability, adoption, and digital literacy affects health outcomes for adults with T2D.
Rationale
It is important for clinicians, public health workers, and policy makers to understand the effects of the Internet and technology on T2D adults’ health outcomes. During the pandemic, data indicate that HbA1c testing for people with diabetes decreased significantly in the United States, glycemic control may have worsened among adults with T2D, medication adherence was negatively impacted, some in-person healthcare services was not available when needed, and physical activity reduced in some populations (10–14). Many of these studies cite Internet availability and digital literacy barriers as a potential factor for these outcomes yet these factors were not directly studied.
Objectives
While the concept of the digital divide is not new, there is limited research examining the association of health outcomes of adults with T2D and disparities in Internet availability and adoption. A scoping review was conducted to better understand the knowledge and research for this topic. The research questions guiding this scoping review are as follows:
- What is known in peer-reviewed scientific articles, written in the English language, published in the last 10 years about health disparities in adults with Type 2 diabetes who have insufficient availability or adoption barriers to the Internet and related technologies?
- What social determinants of health (e.g., inadequate housing, food insecurity, poverty) are reported, if any, within the studies identified that impact nutrition, diabetes prevalence, physical activity, disease self-management, and A1c in adults with Type 2 diabetes?
Methods and Materials
This review follows the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) extension for Scoping Reviews (15). The pre-screening protocol is available here.
Eligibility criteria
Inclusion criteria included peer-reviewed, English language studies published in the last 10 years that include dependent variables of diabetes health outcomes or T2D prevalence with independent variables including Internet/technology availability, Internet adoption, Internet usage, digital health literacy and the adult population. Exclusion criteria included digital health application studies, Type 1 Diabetes only, letters to the editor, pharmacological studies, studies unrelated to diabetes, studies about genetics or biochemistry, theory articles, and reviews.
Information sources
Databases queried included CINAHL (through the EBSCO interface), PubMed, and Scopus. No attempt was made to contact the authors of articles identified. All searches were executed on November 29th, 2023. Gray literature was not used in this review.
Search strategy
PubMed was the first database searched. I used a complex search strategy, with assistance from the University of Missouri Library to formulate the search string. The concepts of digital divide, underserved populations, Internet availability, diabetes, and diabetic outcomes were thoroughly developed with multiple search terms. Embedded within the search are limits for English language, adult population, and publication date in the last 10 years. Search strategy for CINAHL and Scopus were modeled from the PubMed search terms. Full search terms for all data sources are presented in Table 1.
Selection process
All search results were exported to the bibliographic software Zotero (18) version 6.0.30. Results were combined into a single folder to assist with unified export. Results were exported to a spreadsheet containing publication date, author(s), title, abstract, publication title, tags (assigned by Zotero), ISSN, digital object identifier (DOI), and relevant URL links. Duplicates were identified by assessing matched titles, ISSN, and DOI.
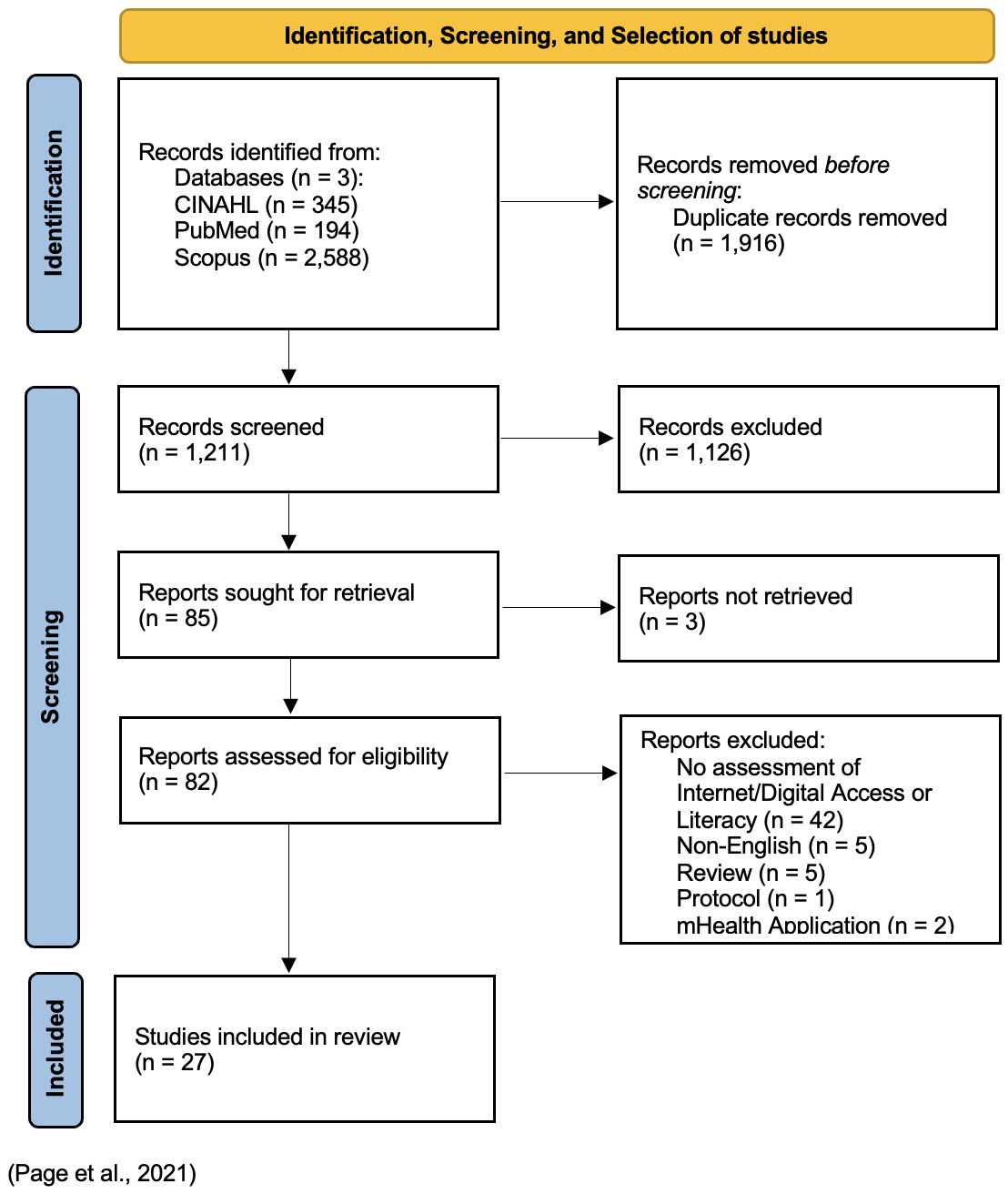
During the screening process, author(s), publication title, keyword tags, ISSN, DOI, and URL were hidden. Screening was executed in three stages. The first stage of screening I assessed the article titles for eligibility criteria. The second stage of screening was a review of the abstract. The final stage of screening utilized full text. All screening was completed manually without the use of automated computer software. During each screening stage, I noted in a “Keep” column on the spreadsheet if the article should be “Y” kept, “N” removed”, or “R” reviewed in subsequent stages if the title or abstract were unclear. Selection process was documented in a PRISMA flow diagram (18).
Data collection process and data items
Data were collected in a review matrix spreadsheet during full text review of each study. Variables collected in the matrix spreadsheet after the screening process included publication date, author(s), title, abstract, digital object identifier (DOI), study objectives, research question(s), study design, population studied, setting, independent variable, dependent variable, sample characteristics, timeframe of study, recruitment/data collection methods, general methods, key findings, limitations, and a relevant summation of the study with key themes.
Syntheses methods and critical appraisal
Syntheses of the evidence was completed by creating individual summaries of the studies. Key themes were identified within the results that align with this review’s research questions. Individual study findings were categorized under thematic elements in final synthesis. The quality of evidence was not systematically appraised. Limitations of the individual articles were reported in the data collection.
Results & Discussion
Study selection
After organizing the studies into the review matrix spreadsheet, 1,916 duplicates were removed, leaving 1,211 articles for title and abstract screening. Title screening resulted in 925 studies that met the exclusion criteria and 286 studies evaluation in abstract screening. Abstract screening yielded 85 articles for full text review. Three articles were unable to be retrieved. Full text was reviewed for 82 articles leading to 54 articles excluded. 27 studies were selected for final analysis. See complete PRISMA flow diagram in Figure 1.
Results of individual studies and syntheses
The full literature matrix including results and syntheses of individual studies is provided in the Supplementary Table S1 and S2.
Article characteristics
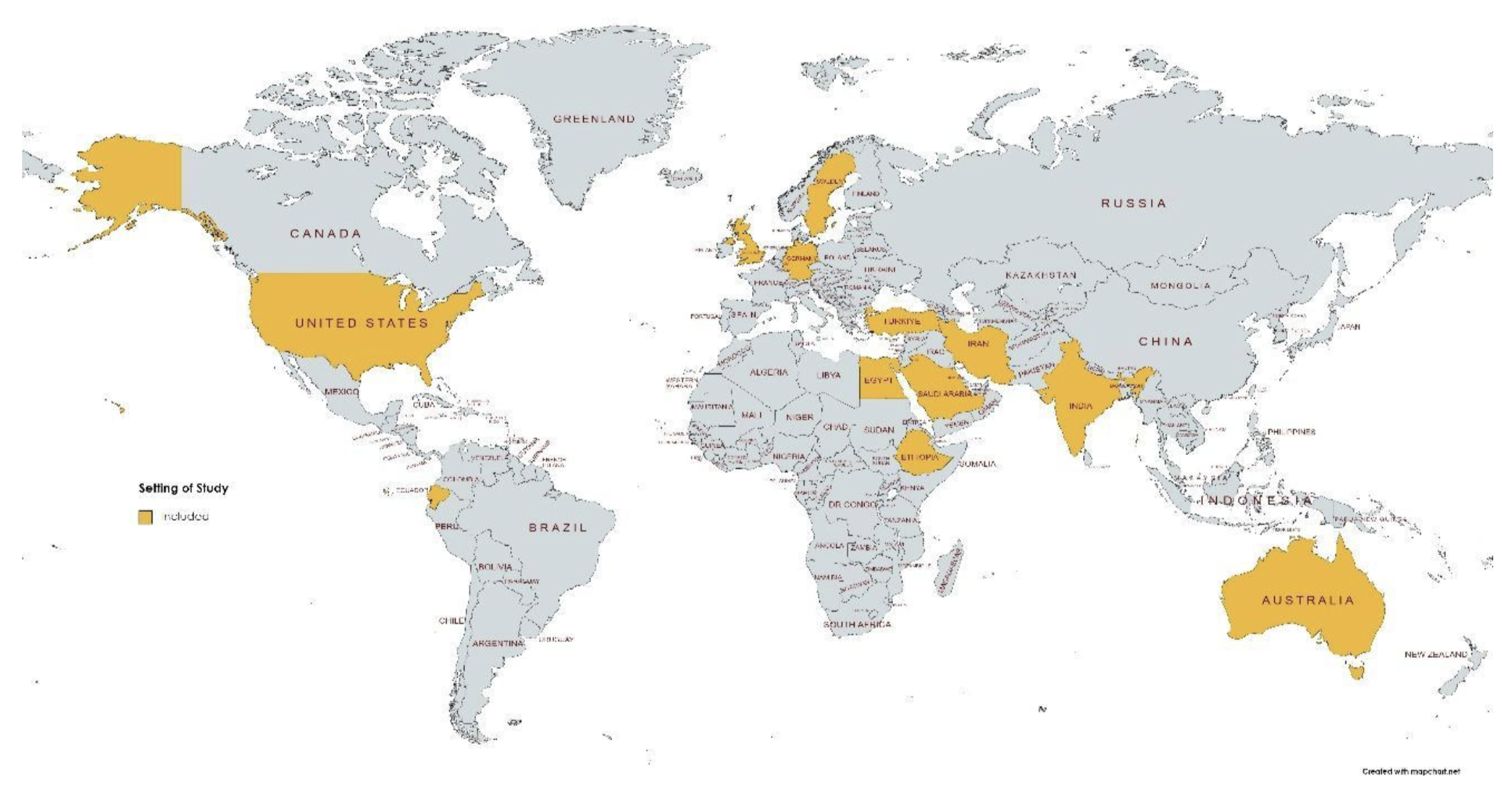
Reviewed studies indicate a heterogeneous range of objectives, study protocols, populations, settings, and sampling. The details of each study are presented in the literature review matrix in Table S1 in the Appendix. Notably, nine studies utilized qualitative methodologies using semi-structured interviews (n=7) and focus groups (n=2). Other studies were quantitative and were primarily observational and cross-sectional. All studies incorporated diabetes prevalence, self-management, clinical outcomes, or disease knowledge in some way through population sampling or data collection methods. Settings included an international assortment of countries within North America, South America, Africa, Europe, Australia, and Asia. See Figure 2 for a geographic representation of the countries included.
Digital divide and health disparities
Digital disparities create challenges in accessing digital health solutions such as telehealth, self-management applications, and patient portals (20–25). For example, Chambers et al. found that only 38.6% of American Indian youth, with high BMI and HbA1c levels had access to the internet, limiting the benefit of digital health solutions. Disparities in eHealth literacy were linked to older adults by Price-Haywood et al, limiting their ability to utilize patient portals. They found that portal users typically were younger and had higher educational attainment.
Additionally, longitudinal data from United States metropolitan and micropolitan statistical areas suggests that Internet adoption is associated with decreased diabetes prevalence and improvements in diabetic risk factors (26). In their longitudinal study, Whitacre and Brooks utilized first-difference modeling of 92 metropolitan and micropolitan statistical areas exploring the impact of Broadband adoption rates on community health outcomes found in the CDC’s Behavioral Risk Factor Surveillance System. They found that adoption is significantly correlated with 9 out of 24 health measures including reduced smoking rates, reduced diabetes prevalence, and increased consumption of fruits and vegetables. While establishing a quantitatively significant correlation of Internet adoption’s effect on health outcomes, the results of this study were limited by not assessing online behaviors and Internet-connected smartphone adoption.
Individuals with limited Internet availability and digital literacy, notably older adults and rural inhabitants, face significant disadvantages in managing chronic conditions like diabetes (27,28). The complexity of chronic disease management, poor healthcare access, and affordability of the Internet and associated technologies compound this problem. Across many countries, educational attainment and income positively impact the rates of adoption of the Internet and related technology (24,25,29–34).
Health information-seeking behaviors
Race and ethnicity appears to affect health information-seeking behaviors (HISB) across diverse populations. American Indian and Alaska Native adults demonstrated high rates of Internet adoption (81%) and expressed openness to online nutrition education, with most accessing the Internet through smartphones (67%) and family members (90%) (36). Young Punjabi Sikhs in the United Kingdom preferred Internet-based diabetes information over healthcare professionals, citing convenience and perceived gaps in cultural awareness among providers (35). African American veterans, while having access to technology, reported that sociocultural factors and past experiences with healthcare institutions influenced their adoption of digital health tools (37). Studies in Iran, Egypt, and Ecuador revealed varying patterns of technology use among different ethnic groups, highlighting the need for culturally sensitive digital health interventions (22, 29, 46).
Systemic and infrastructural barriers were not specifically associated with HISB but were apparent in the review. There are significant disparities in internet availability, across multiple regions and countries, with rates varying from 27.2% in Ecuador to 90% in Iran (29,39). In the southeastern United States, counties with lower Internet availability showed higher diabetes prevalence (43).
Individual attitudes and capabilities influenced HISB, with multiple studies highlighting the role of age, education, and digital literacy. Research in Turkey found that only 34.8% used the Internet for health information, with usage correlated to younger age and higher educational status (33). Weymann et al. showed that 61.7% of German participants used the Internet for health information, while 35.1% of non-users cited lack of Internet access as the primary barrier (41). In Ethiopia, while willingness to use mHealth applications was high (71.4%), actual adoption remained low (13.1%), related to factors such as digital literacy and perceived ease of use (28).
Technology use and health literacy
There is strong adoption of mobile phones in many populations which allows access to mHealth services and health information but higher educational status and financial affluence appear to positively influence mobile phone adoption (27–29,36–38). Despite the potential for digital health services to facilitate diabetes self-care management, barriers such as financial limitations, digital literacy, and poor Internet availability persist. Those with limited adoption of digital technology faced greater challenges in understanding medical conditions and education from healthcare providers than their connected peers, suggesting that technology has a relationship with health literacy levels (21,25,38–40).
Social determinants of health
In the studies reviewed, access to and adoption of the Internet is linked with dependencies to educational attainment, income, and geographic location (21, 24, 25 ,27-34, 36-40). For example, Cherrez-Ojeda et al. found 45.2% of Ecuadorian diabetes patients used the Internet to find diabetes information but Internet access was associated with higher income and higher education levels. Umeh et al. reported that residents of the UK with a computer at home was associated with higher socioeconomic status. Furthermore, data from the Veteran’s Affairs health system indicated that rural patients relied more on in-person care during the pandemic which Yoon et al. suggest is due to Internet availability. Despite greater availability of Internet access in non-rural areas, Fuji et al. report that financial barriers impact usage of online personal health records in their metropolitan-area study. These studies echo findings by the National Telecommunications and Information Administration who estimate that 18.2 million households have not adopted broadband internet with population characteristics of non-adopters were those making less than $25,000 per year, people of color, or had lower educational attainment (8). Only one study explored the association between food insecurity, Internet availability, and diabetes prevalence within the results (43). Sharma applied a socio-ecological perspective in Southeastern US states, finding that food insecurity and Internet availability were strongly linked to diabetes prevalence at the county-level. Other social determinants such as housing, transportation, health care access, health insurance, employment, and social support systems were not reported in these studies.
Summary of evidence
The evidence provided from these sources indicates an evolving qualitative and quantitative understanding of the digital divide, health disparities, health information-seeking behaviors, technology use, health literacy. Regarding social determinants of health, 16 of the 27 studies link educational attainment, income, and geographic location as significant factors in access and adoption of the Internet and related technologies. While the studies accessed do not directly answer the question of the behaviors and diabetes outcomes associated with social determinants, the linkage can be made through existing reviews, that access and adoption are a predictive factor for usage of digital personal health records potentially impacting the ability for providers to share timely health information to remote patients (47).
Limitations
First, the international and heterogenous mixture of qualitative and cross-sectional quantitative data limits the findings of this review and presents challenges in a concluding synthesis. This presents a limitation for this review but also reveals the limited knowledge in this area. Second, the inclusion and exclusion criteria must be contextualized in this review. The adherence to the inclusion criteria of the English language may have limited the inclusion of significant research conducted in other languages. The exclusion of gray literature may omit data and insights that could enrich the understanding of the complexities of Internet availability, adoption, and digital literacy. Third, factors such as cultural beliefs, health care policy, and economic infrastructure were not directly studied which leads to an incomplete understanding of the multi-layered nature of health disparities and the digital divide. Fourth, a critical appraisal and meta-analysis were not conducted on the obtained articles. Robust reviews such as meta-analysis are needed as more research is conducted in this domain. Lastly, the research reviewed here is limited to November 29th, 2023. Additional studies in this domain have been published, requiring an additional review.
Conclusions
These studies suggest a persistent digital divide that includes inadequate Internet availability, limited Internet adoption in some populations, poor digital and health literacy, and socioeconomic barriers that impact the knowledge and management of T2D. Evidence directly linking Internet adoption to diabetes prevalence is limited to a single study (26). The Internet and digital health technologies can be leveraged to educate and empower individuals and providers to manage diabetes more effectively but disparities in education, income, and cultural norms must be considered. Future research should further explore the relationship of Internet availability, Internet adoption, social determinants of health, and digital health services on health outcomes related to diabetes in more populations within the United States and internationally.
Acknowledgments
Not applicable.
Author Contributions
MF is responsible for all contributions to this article.
Data Availability
Pre-screening file and the data collection matrix are available here.
Supplemental Information
Supplemental information is available here.
Transparent Peer Review
Results from the Transparent Peer Review can be found here.
Recommended Citation
Farmer, M.S. (2025). A scoping review of internet access, digital literacy, and health outcomes in adults with Type 2 diabetes. Stacks Journal: 25004. https://doi.org/10.60102/stacks-25004
References
- World Health Organization. World Health Organization. 2021 [cited 2023 Oct 18]. Global strategy on digital health 2020-2025. Available from: https://iris.who.int/bitstream/handle/10665/344249/9789240020924-eng.pdf?sequence=1&isAllowed=y
- Boniol M, Kunjumen T, Nair TS, Siyam A, Campbell J, Diallo K. The global health workforce stock and distribution in 2020 and 2030: a threat to equity and ‘universal’ health coverage? BMJ Glob Health. 2022 Jun 1;7(6):e009316.
- Zhang X, Lin D, Pforsich H, Lin VW. Physician workforce in the United States of America: forecasting nationwide shortages. Hum Resour Health. 2020 Feb 6;18:8.
- Crawford A, Serhal E. Digital health equity and covid-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. 2020;22(6).
- Early J, Hernandez A. Digital disenfranchisement and covid-19: broadband internet access as a social determinant of health. Health Promot Pract. 2021 Sep;22(5):605–10.
- Kruse RL, Koopman RJ, Wakefield BJ, Wakefield DS, Keplinger LE, Canfield SM, et al. Internet use by primary care patients: where is the digital divide? Fam Med. 2012;44(5):342–7.
- Robotham D, Satkunanathan S, Doughty L, Wykes T. Do we still have a digital divide in mental health? a five-year survey follow-up. J Med Internet Res [Internet]. 2016;18(11). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84996636657&doi=10.2196%2fjmir.6511&partnerID=40&md5=a2b973ac392b995a241b3f1dbc6aeb47
- NTIA. Switched Off: Why Are One in Five U.S. Households Not Online? | National Telecommunications and Information Administration. 2021. Accessed January 2, 2024. https://www.ntia.gov/blog/2022/switched-why-are-one-five-us-households-not-online
- Turnbull S, Lucas PJ, Hay AD, Cabral C. The role of economic, educational and social resources in supporting the use of digital health technologies by people with t2d: a qualitative study. BMC Public Health. 2021 Feb 5;21(1):293.
- Czeisler MÉ, Barrett CE, Siegel KR, Weaver MD, Czeisler CA, Rajaratnam SMW, et al. Health care access and use among adults with diabetes during the covid-19 pandemic – united states, february-march 2021. MMWR Morb Mortal Wkly Rep. 2021 Nov;70(46):1597–602.
- Eberle C, Stichling S. Impact of covid-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: a systematic review. Diabetol Metab Syndr. 2021 Sep 7;13(1):95.
- Fadini GP, Bonora BM, Morieri ML, Avogaro A. Why diabetes outpatient clinics should not close during pandemic crises. J Endocrinol Invest. 2021 Jan;44(8):1795–8.
- Fragala MS, Kaufman HW, Meigs JB, Niles JK, McPhaul MJ. Consequences of the covid-19 pandemic: reduced hemoglobin a1c diabetes monitoring. Popul Health Manag. 2021 Feb;24(1):8–9.
- Ratzki-Leewing AA, Ryan BL, Buchenberger JD, Dickens JW, Black JE, Harris SB. Covid-19 hinterland: surveilling the self-reported impacts of the pandemic on diabetes management in the usa (cross-sectional results of the inphorm study). BMJ Open. 2021 Sep 2;11(9):e049782.
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. Prisma extension for scoping reviews (prisma-scr): checklist and explanation. Ann Intern Med. 2018 Oct 2;169(7):467–73.
- Alessi J, Becker AS, Amaral B, de Oliveira GB, Franco DW, Knijnik CP, et al. Type 1 diabetes and the challenges of emotional support in crisis situations: results from a randomized clinical trial of a multidisciplinary teleintervention. Sci Rep [Internet]. 2022;12(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85125157385&doi=10.1038%2fs41598-022-07005-w&partnerID=40&md5=b06c47ca64ee9ba6be5e3333dd4a9adf
- Padhy S, Dash S, Routray S, Ahmad S, Nazeer J, Alam A. IoT-Based Hybrid Ensemble Machine Learning Model for Efficient Diabetes Mellitus Prediction. Comput Intell Neurosci [Internet]. 2022;2022. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85131218784&doi=10.1155%2f2022%2f2389636&partnerID=40&md5=ab58aaefe0e8aa2124a537cee7b05a45
- Zotero [Internet]. [cited 2023 Nov 30]. Available from: https://www.zotero.org/
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71.
- Chambers RA, Rosenstock S, Neault N, Kenney A, Richards J, Begay K, et al. A Home-Visiting Diabetes Prevention and Management Program for American Indian Youth: The Together on Diabetes Trial. Diabetes Educ. 2015 Dec;41(6):729–47.
- Fuji KT, Abbott AA, Galt KA. A qualitative study of how patients with type 2 diabetes use an electronic stand-alone personal health record. Telemed J E-Health Off J Am Telemed Assoc. 2015 Apr;21(4):296–300.
- Mansour E. An Investigation into the Information-Seeking Behavior of Egyptian Adult Patients with Type 2 Diabetes Mellitus (T2DM). J Hosp Librariansh. 2021 Oct;21(4):367–90.
- Pettersson S, Jaarsma T, Hedgärd K, Klompstra L. Self-care in migrants with type 2 diabetes, during the COVID-19 pandemic. J Nurs Scholarsh. 2023;55(1):167–77.
- Price-Haywood EG, Harden-Barrios J, Ulep R, Luo Q. eHealth literacy: Patient engagement in identifying strategies to encourage use of patient portals among older adults. Popul Health Manag. 2017 Dec;20(6):486–94.
- Ramasamy D, Singh AK, Mohan SK, Meenakshi N. Association of sociodemographics, technology use and health literacy among Type 2 diabetic individuals living in an Indian setting: An exploratory cross-sectional study. Int J Diabetes Dev Ctries. 2016;36(3):303–12.
- Whitacre B, Brooks L. Do broadband adoption rates impact a community’s health? Behav Inf Technol. 2014 Jul;33(7):767–79.
- Kim KK, Mcgrath SP, Solorza JL, Lindeman D. The ACTIVATE Digital Health Pilot Program for Diabetes and Hypertension in an Underserved and Rural Community. Appl Clin Inform. 2023;14(4):644–53.
- Walle AD, Ferede TA, Shibabaw AA, Wubante SM, Guadie HA, Yehula CM, et al. Willingness of diabetes mellitus patients to use mHealth applications and its associated factors for self-care management in a low-income country: An input for digital health implementation. BMJ Health Care Inform [Internet]. 2023;30(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85160379058&doi=10.1136%2fbmjhci-2023-100761&partnerID=40&md5=e909eee1485f86bb308dd956b2eabdc1
- Chérrez-Ojeda I, Vanegas E, Calero E, Plaza K, Cano JA, Calderon JC, et al. What Kind of Information and Communication Technologies Do Patients with Type 2 Diabetes Mellitus Prefer? An Ecuadorian Cross-Sectional Study. Int J Telemed Appl [Internet]. 2018;2018. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85062822663&doi=10.1155%2f2018%2f3427389&partnerID=40&md5=459af10c33665dd17c7eb8158d3edf50
- Jemere AT, Yeneneh YE, Tilahun B, Fritz F, Alemu S, Kebede M. Access to mobile phone and willingness to receive mHealth services among patients with diabetes in Northwest Ethiopia: A cross-sectional study. BMJ Open [Internet]. 2019;9(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85060515808&doi=10.1136%2fbmjopen-2018-021766&partnerID=40&md5=dfdaec377c2e86cfa771ad85682d58ae
- Samadbeik M, Garavand A, Saremian M, Baraei Z, Adeli M. Readiness of patients with chronic diseases to use health information technology: An experience of a developing country. Shiraz E Med J [Internet]. 2018;19(10). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85056430598&doi=10.5812%2fsemj.65797&partnerID=40&md5=5256923c1408d18723f081ffca0eff81
- Taibah H, Arlikatti S, Delgrosso B. Advancing e-health in Saudi Arabia: Calling for smart village initiatives. WIT Trans Ecol Environ. 2020;249:261–74.
- Terkeş N, Çelik F, Bektaş H. Determination of the Technology Use Status and Attitudes Towards Technology of Patients with Type 2 Diabetes. Cyprus J Med Sci. 2022 Oct;7(4):477–83.
- Umeh K, Mackay M, Le-Brun SD. Ethnic differences in diabetes prevalence and ICT use. Br J Nurs. 2015;24(20):1017–23.
- Sidhu T, Lemetyinen H, Edge D. ‘Diabetes doesn’t matter as long as we’re keeping traditions alive’: a qualitative study exploring the knowledge and awareness of Type 2 diabetes and related risk factors amongst the young Punjabi Sikh population in the UK. Ethn Health. 2022;27(4):781–99.
- Stotz S, Brega AG, Lockhart S, Hebert LE, Henderson JN, Roubideaux Y, et al. An online diabetes nutrition education programme for American Indian and Alaska Native adults with type 2 diabetes: perspectives from key stakeholders. Public Health Nutr. 2021 Apr;24(6):1449–59.
- Johnson NL. Towards Understanding Disparities in Using Technology to Access Health Care Information: African American Veterans’ Sociocultural Perspectives on Using My HealtheVet for Diabetes Management. Health Commun. 2023 Oct;38(11):2399–407.
- Nguyen KH, Cemballi AG, Fields JD, Brown W, Pantell MS, Lyles CR. Applying a socioecological framework to chronic disease management: implications for social informatics interventions in safety-net healthcare settings. JAMIA Open [Internet]. 2022;5(1). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85142105608&doi=10.1093%2fjamiaopen%2fooac014&partnerID=40&md5=806afcbd029b9a5754543dc5a79571c0
- Rastegari H, Schulz PJ, Kamali M, Nasrollahi A. Assessing Health Literacy and Communication Skills in Medical Referrals: A Survey Study. J Health Lit. 2022;7(3):37–52.
- Yom-Tov E, Marino B, Pai J, Harris D, Wolf M. The Effect of Limited Health Literacy on How Internet Users Learn About Diabetes. J Health Commun. 2016 Oct;21(10):1107–14.
- Weymann N, Härter M, Dirmaier J. Information and decision support needs in patients with type 2 diabetes. Health Informatics J. 2016;22(1):46–59.
- Yoon J, Chen C, Chao S, Wong E, Rosland AM. Adherence to Diabetes Medications and Health Care Use during the COVID-19 Pandemic among High-Risk Patients. J Am Board Fam Med. 2023;36(2):289–302.
- Sharma A. Exploratory spatial analysis of food insecurity and diabetes: an application of multiscale geographically weighted regression. Ann GIS [Internet]. 2023; Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85159366423&doi=10.1080%2f19475683.2023.2208199&partnerID=40&md5=f1d0c0090e4a96c6903603cd8fc10133
- Hincapie AL, Gupta V, Brown SA, Metzger AH. Exploring Perceived Barriers to Medication Adherence and the Use of Mobile Technology in Underserved Patients With Chronic Conditions. J Pharm Pract. 2019;32(2):147–53.
- Dao J, Spooner C, Lo W, Harris MF. Factors influencing self-management in patients with type 2 diabetes in general practice: a qualitative study. Aust J Prim Health. 2019 Mar;25(2):176–84.
- Talebian A, Borhani F, Okhovati M. A grounded theory study on health information seeking behavior of Iranian diabetic. J Kerman Univ Med Sci. 2021;28(1):10–20.
- Abd-alrazaq AA, Bewick BM, Farragher T, Gardner P. Factors that affect the use of electronic personal health records among patients: A systematic review. International Journal of Medical Informatics. 2019;126:164-175. doi: https://doi.org/10.1016/j.ijmedinf.2019.03.014
Open Access
Peer-Reviewed
Creative Commons
Submitted: 31 May 2024
Accepted: 24 March 2025
Published: 28 April 2025
Funding Information: This study received no funding.
Conflicts of Interest: The author declares no conflicts of interest.
© 2025 Farmer. Stacks Journal